"To believe in the things you can see and touch is no belief at all. But
to believe in the unseen is both a triumph and a blessing."
- Bob Proctor
Hemispatial Inattention (Visual Neglect)
Hemispatial inattention is an attention disorder that prevents the patient from attending to stimuli on one side. While it can happen to either the right or the left side, it usually only becomes a clinical problem when the right hemisphere of the brain is damaged and the patient is unable to attend to the left side of the world. It is quite variable in presentation and is more likely a set of problems rather than one specific condition.
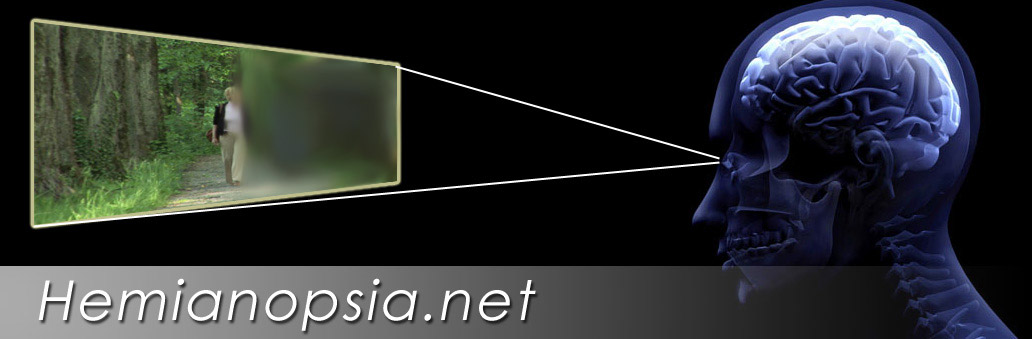
It is a problem that is often confused with homonymous hemianopsia. Hemispatial inattention may occur with or without a homonymous hemianopsia. While homonymous hemianopsia is a physical loss of visual field to the same side in both eyes, visual neglect is an attention problem to one side of their body. We can divide patients into three groups; those with a homonymous hemianopsia and no hemispatial inattention; those with hemispatial inattention only (no hemianopsia) and, those with both homonymous hemianopsia and hemispatial inattention. It is important to determine the status of the neglect versus field loss so that proper treatments can be initiated.
Hemispatial inattention is more than a visual condition, a patient with hemispatial inattention may not respond to a voice when the person is on the left side and may not be able to recall memories of objects or places that would normally be to his left in a specific situation. A man with hemispatial inattention may only shave one side of his face while a patient with only a hemianopsia would compensate by turning his head and eyes to shave both sides of his face. These problems can relate to brain injury in different areas, but are often associated with damage in the right parietal lobe of the brain. The patient may or may not have a loss of visual field, but due to the left hemispatial in-attention cannot learn to compensate because they cannot mentally attend to left side.
Visual neglect usually indicates a worse outcome. Over time the natural course for visual neglect is to slowly improve, but outcomes are quite variable. An 18 month period has been suggested, but results are variable. Occupational therapy may improve outcomes in many patients and visual field expanders may have potential to help in some cases.
Severe hemispatial inattention can be suspected by gross observation alone. The subtle forms can be less obvious, but more crucial for patients with mild neglect who may be attempting to fully reintegrate into the world again including desires to drive or return to work which are situations where even mild hemi-spatial in-attention could be dangerous.

Hemispatial inattention is initially screened for by a combination of patient behavior observations and several basic tests particular drawing tasks. An important screening tool is the Behavioral In-attention Test (BIT). The BIT has six sub tests.
The Daisy drawing above is one small part of the six subtests of the BIT. Here the patient draws only petals on the right side. It suggests hemispatial inattention to the left visual field. This would not happen in hemianopsia alone.

The Letter Cancellation Test , a subtest of the BIT, viewed here shows the patient only crossing out the letters on the far right. This shows an inattention to the left side.
In a Modified Clock Dial Test below, the patient wrote the numbers only on the right side of the clock face. This may not be specific to visual neglect, but should indicate concerns related to visual field and visual spatial perception. It indicates a need to test further for visual neglect.
While we do not yet have adequate studies to fully understand if visual field expansion is effective as a treatment for hemispatial inattention, our experience however, has shown that in some patients with left visual neglect and homonymous hemianopsia together, significant benefit has been demonstrated from visual field expanding devices like the Gottlieb Visual Field Awareness System, the EP Horizontal lens or the Chadwick Hemianopsia Lens.
Please refer to the patient stories of Stacey and Paul. These patients both have homonymous hemianopsia and and left hemispatial inattention and showed dramatic improve with visual field expansion systems. Stacey wears a Gottlieb VFAS and Paul, now deceased, wore a press-on version in the round Gottlieb-like form.
I remember one incident with Stacey that reinforced to me of how much her Gottlieb VFAS helped her left hemispatial inattention. She had been successfully wearing her system for many years. We were about shoot a video with Stacey for a  Breakthroughs in Science television segment in the following week when she broke her eyewear. She wore them in to our office to leave them for the repair. Her mother had driven her to our office in Indianapolis and Stacey had traveled through the building up the elevator and down two intersecting hallways to our office with no problem. She left the system and our office, but soon returned to ask for someone to help her back to her mother’s car. This was obviously a left hemispatial inattention problem as a patient with years of having a left homonymous hemianopsia could adequately compensate for the task of returning to the car.
Breakthroughs in Science television segment in the following week when she broke her eyewear. She wore them in to our office to leave them for the repair. Her mother had driven her to our office in Indianapolis and Stacey had traveled through the building up the elevator and down two intersecting hallways to our office with no problem. She left the system and our office, but soon returned to ask for someone to help her back to her mother’s car. This was obviously a left hemispatial inattention problem as a patient with years of having a left homonymous hemianopsia could adequately compensate for the task of returning to the car.
Unfortunately, a large portion of patients with hemispatial inattention may not respond to visual field expanders. Because we are dealing with a variable condition or group of conditions. Hopefully, we can eventually better understand which patients may respond to visual field expansion and if there is a difference in the type of lens that works best. The Gottlieb VFAS and Chadwick Hemianopsia lenses are dependent on some degree of mild eye scanning movements, which are often severely impaired in these patients. In the EP Horizontal lens, eye movements are not as crucial as there is a  Press-on EP Style Test Lens continuous presentation of the left field above and below the line of sight.
Press-on EP Style Test Lens continuous presentation of the left field above and below the line of sight.
This lens might be more effective in making the visual neglect patient more aware of the left side. Studies are needed to determine if the EP Horizontal lens has potential to help neglect patients.
The EP Horizontal can be tested first with a trial period of wearing a 40 prism diopter press-on mounted across the top of the lens on the left side to determine if the patient will respond. A lower prism segment may also be considered. Then an EP Horizontal Lens can be considered or in some cases the press-on lens may be continued. If no improvements occurs in the 6 to 12 weeks, the press-on lens can be removed. Hemispatial inattention patients frequently benefit from occupational therapy to learn to attend the affected side. Any optical treatments should be combined with occupational therapy.
Extinction
Patient may report that they cannot see something move on the left side if their attention is directed to the right side. They may likewise feel a touch on the left side, but not if the right side is touched simultaneously. It appears that the stimuli on the right whether visual, auditory or tactile overwhelms the attention system suppressing the opposite side. Extinction may represent a mild form of visual neglect. It is often masked and thus undetectable when significant neglect is present, but may emerge as the patient recovers from the visual neglect.
In the movie above, a patient with an acquired brain injury for several years demonstrates extinction. Note that he is able to feel a touch on either shoulder, but not on the left side when his right shoulder is tapped simultaneously.
Anosognosia
Patients with hemispatial inattention may frequently deny that they have a problem. In the examination room, patients tell us they have no problem to the left and never run into things, but their spouse or caregiver may quickly report that the patient is constantly running into things, tripping and being startled.
 The most famous case of anosognosia was President Woodrow Wilson. After suffering two strokes in the right posterior hemisphere, he developed left hemispatial inattention and a left homonymous hemianopsia. When colleagues came to visit him, he failed to respond to them until they were escorted to his right side. He denied he had a problem and planned to run for a third term as president until his wife finally intervened.
The most famous case of anosognosia was President Woodrow Wilson. After suffering two strokes in the right posterior hemisphere, he developed left hemispatial inattention and a left homonymous hemianopsia. When colleagues came to visit him, he failed to respond to them until they were escorted to his right side. He denied he had a problem and planned to run for a third term as president until his wife finally intervened.
Frequently, we see patients who by the report of their spouse are doing much better since the field expander trial with a press-on was initiated, but the patient insists the field expander is making no difference. In one case in particular the patient said he had no problems in his vision and demanded the press-on field expander be removed immediately. After failing to convince him to continue with it for a longer period of time, I removed it. He started to walk out of the examination room and crashed to the left door-frame. Fortunately, he returned, sat down and said, “Put it back on!”
Our experience tells us to discuss the functioning of these patients with both the patient and the caregiver. Do not rely entirely on what the patients report if your observation and the caregiver observations differ. Try to get the patient to stay with the system long enough for real behavioral patterns to be observed.
Please contact us if you have any questions.
The Low Vision Centers of Indiana
Richard L. Windsor, O.D., F.A.A.O., D.P.N.A.P.
Craig A. Ford, O.D., F.A.A.O.
Laura K. Windsor, O.D., F.A.A.O.
Ali E. Prible, O.D.
Indianapolis (317) 844-0919
Fort Wayne (260) 432-0575
Hartford City (765) 348-2020